
[ad_1]
High rates of false positive test results may be keeping women from sticking to recommended mammogram screenings for breast cancer, a new study has found.
Researchers from UC Davis Comprehensive Cancer Center in Sacramento, California, reviewed more than 3.5 million screening mammograms performed among more than one million women between 2005 and 2017.
Women who received a true-negative result were more likely to return for future screenings, with a 77% compliance rate.
THESE 17 CANCER TYPES ARE MORE COMMON IN GEN X AND MILLENNIALS, AS STUDY NOTES ‘ALARMING TREND’
By comparison, among those who received a false positive, only 61% returned for another mammogram in six months, and 67% returned for a recommended biopsy. (A false positive occurs when a mammogram shows an abnormal result that is investigated further, but does not lead to a cancer diagnosis.)
The women, who ranged in age from 40 to 73, had not previously received a breast cancer diagnosis.

High rates of false positives may be keeping women from sticking to recommended mammogram screenings for breast cancer, a new study has found. (iStock)
The study findings were published in the Annals of Internal Medicine on Sept. 3.
Surprising findings
“We found that women were less likely to return for another screening mammogram if they were recalled for additional imaging that did not result in a cancer diagnosis, especially if that recall resulted in a recommendation for a short-interval follow-up or biopsy or if they experienced false-positive exams on two consecutive screening mammograms,” lead study author Dr. Diana Miglioretti, a professor and division chief of biostatistics in the UC Davis School of Medicine’s Department of Public Health Sciences, told Fox News Digital.
SENIORS AND BREAST CANCER: WHY AREN’T OLDER WOMEN TOLD TO GET MAMMOGRAMS?
Miglioretti said she was surprised by the findings, as surveys have suggested that women believe they would be just as likely to continue screening even after a false-positive result.
“However, something about the experience seems to influence their actual behavior, and despite their intentions to return, some do not,” she added.
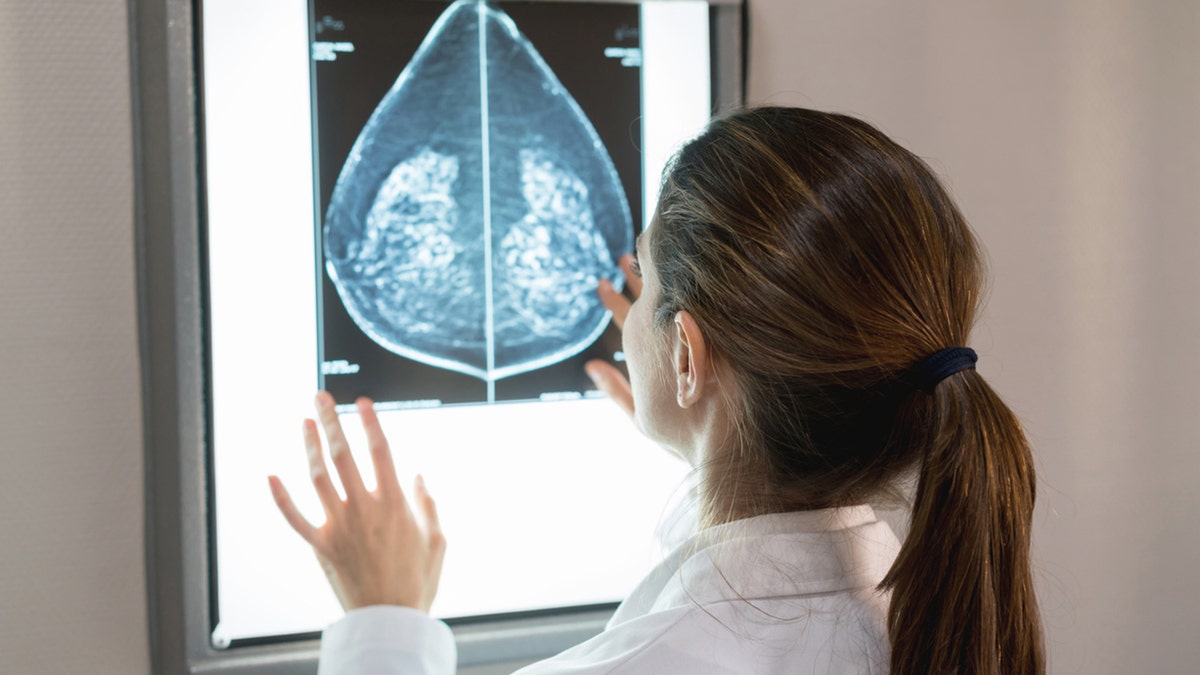
A false positive occurs when a mammogram shows an abnormal result that is investigated further, but does not lead to a cancer diagnosis. (iStock)
Another surprising element, Miglioretti said, was that a false-positive recommendation for a short-interval follow-up — meaning the patient needs to return in six months for diagnostic imaging to evaluate changes in the abnormal finding — had the greatest impact on a woman’s likelihood of not returning for future screenings.
“I initially expected that the probability of returning would be lowest for those who had undergone a benign biopsy,” she said.
“Approximately 10% of screening mammograms require diagnostic work-up, and most women called back for further imaging do not have breast cancer.”
“However, even after following women for five years after a false-positive result, women who received a short-interval follow-up recommendation were the least likely to return for future screening mammograms.”
Asian and Hispanic/Latinx women were least likely to return for future screenings after a false positive.
BREAST CANCER MAMMOGRAM SCREENINGS SHOULD START AT AGE 40 INSTEAD OF 50, SAYS HEALTH TASK FORCE
“This is extremely concerning, as recent trends have conveyed a much faster rate of growth in breast cancer rates in this demographic than in other ethnic and racial groups,” Dr. Tingting Tan, MD, PhD, a medical oncologist and hematologist at City of Hope Newport Beach in California, told Fox News Digital.
(Tan was not involved in the study.)
“There is a 52% rise in breast cancer rates in the last two decades among Asian-American and Pacific Islander women under the age of 50.”
What to know about false positives
A false positive occurs when a mammogram shows an abnormal result that is investigated further, but does not lead to a cancer diagnosis.
“Following the mammogram, the results will either come back as clear (known as a true negative) or will be flagged for additional testing,” Tan said.

Some common causes of false positives include dense breast tissue, small calcium deposits in the breast, overlapping breast tissue that creates shadows or normal variations in breast tissue. (iStock)
Some common causes of false positives, according to UC Davis, include dense breast tissue, small calcium deposits in the breast, overlapping breast tissue that creates shadows, or normal variations in breast tissue.
False-positive results occur in 10% to 12% of mammograms for women between 40 and 49 years of age, UC Davis noted.
SOME BREAST CANCER PATIENTS COULD BE AT RISK OF ANOTHER TYPE OF CANCER, STUDY REVEALS
Within a decade of annual screenings, up to 60% of women experience at least one false positive result.
As a breast cancer specialist, Tan said she often hears the term “scanxiety” to describe the fear that is associated with imaging.
“Even a slight possibility of being diagnosed with cancer can be debilitating, and we understand that the follow-up check-ups after an abnormal mammogram can take an emotional toll,” she said.

“If women have concerns about their false-positive result or are unclear of what it means, they should talk with their doctor,” an expert advised. (iStock)
“While it can be distressing to not have a true negative from that initial mammogram, patients should not worry if their doctor orders a breast ultrasound following a mammogram, as it is a very common procedure.”
Asking questions and having open communication with health care providers can help to ease stress and anxiety when there is follow-up to an abnormal screening, Tan added.
Importance of continued screenings
Based on these findings, the researchers emphasized that women who receive false-positive results should continue screening every one to two years.
“A false positive — particularly if it leads to a diagnosis of benign breast disease — is associated with a small increase in developing breast cancer in the future,” Miglioretti said.
CLICK HERE TO GET THE FOX NEWS APP
“If women have concerns about their false-positive result or are unclear of what it means, they should talk with their doctor.”
Women should also be aware that a screening test often requires further diagnostic evaluation to confirm that a finding is normal, the doctor added.
“A false positive — particularly if it leads to a diagnosis of benign breast disease — is associated with a small increase in developing breast cancer in the future.”
“This is a standard part of the screening process,” Miglioretti told Fox News Digital.
“Approximately 10% of screening mammograms require diagnostic work-up, and most women called back for further imaging do not have breast cancer.”
Tan emphasized the importance of mammograms as the “gold standard” for breast screening.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
“Mammograms can catch cancer at early stages, before symptoms,” she told Fox News Digital.
“They are proven to decrease mortality, which is why almost every patient will begin with a screening mammogram.”
Potential limitations of the study
The researchers only evaluated false positives on the two prior screening mammograms for each woman, the researchers noted.

“Cancer is highly complex, and it is essential to see a radiologist who specializes in reading mammograms,” an expert advised. (iStock)
“Women could have had false-positive mammograms prior to that,” Miglioretti noted.
The study was also limited to 177 facilities participating in the Breast Cancer Surveillance Consortium (BCSC), which means some women could have received care at non-BCSC facilities.
For more Health articles, visit www.foxnews.com/health
“Cancer is highly complex, and it is essential to see a radiologist who specializes in reading mammograms,” Tan advised.
“Early detection is key for better outcomes, which is why it is so important to know your breast cancer risk and to get your regular screenings.”
[ad_2]
Source link